Prior Authorization: U.S. Insurers Simplify Care Approval
Prior authorization has emerged as a pivotal topic in the evolving landscape of U.S. healthcare changes, highlighting the ongoing efforts by health insurers to reform the insurance approval process. Major U.S. health insurers, including CVS Health and UnitedHealthcare, have reacted to significant criticism and are taking steps towards simplifying healthcare processes associated with care approvals. This initiative is not just about efficiency; it’s an essential part of the broader movement towards patient care improvement, recognizing that delays in access can have serious health implications. As these insurers strive to reduce the burdens of prior authorization, they aim to connect millions of Americans with necessary treatments more quickly. The anticipated changes may lead to a transformational shift in how patients interact with their insurers and healthcare providers in the coming years.
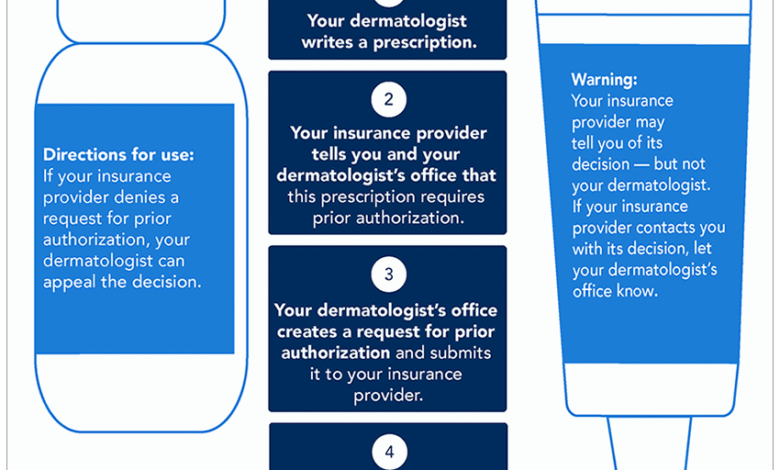
The term “care approval process” often surfaces in discussions around prior authorization, synonymous with the administrative hurdles many face within healthcare systems. Essentially, this process demands that healthcare professionals obtain permission from insurance providers before proceeding with specific treatments or services. This has been a controversial topic as it complicates the delivery of timely care, leading to delays that can jeopardize patient outcomes. Many in the healthcare industry advocate for a streamlined insurance approval process, emphasizing the necessity of making healthcare more accessible and efficient. By addressing these challenges, health insurers are working towards simplifying the experience for both patients and providers alike.
Understanding Prior Authorization in Healthcare
Prior authorization is a critical component of the healthcare system that requires healthcare providers to obtain approval from insurance companies before certain treatments or medications can be administered. This process is intended to ensure that care is medically necessary and appropriate, thereby controlling costs for health insurers. However, prior authorization has often been criticized for hindering timely access to care for patients, leading to delays that can adversely affect health outcomes. As healthcare continues to evolve, the reform of prior authorization processes is crucial to improving patient experiences and outcomes.
The newly announced commitment from major U.S. health insurers to simplify prior authorization aims to address these challenges. Insurers like Cigna and UnitedHealthcare are actively working to expedite approval timelines and minimize the bureaucratic hurdles that often frustrate both patients and healthcare providers. By streamlining these processes, the hope is to enhance patient care improvement across the board and reduce the burden associated with navigating insurance approval.
Frequently Asked Questions
What is prior authorization in healthcare and why is it important?
Prior authorization is a mandatory process where healthcare providers must obtain approval from a patient’s health insurer before performing certain medical services or prescribing specific medications. This process is crucial because it helps insurance companies control costs and ensure that patients receive appropriate and necessary care, although it has been criticized for creating barriers to timely patient treatment.
How are U.S. health insurers reforming the prior authorization process?
Major U.S. health insurers, including CVS Health, UnitedHealthcare, and Cigna, have announced plans to reform the prior authorization process by streamlining procedures and reducing delays in care. These reforms aim to simplify healthcare processes for patients and providers, making it easier to secure approval for necessary treatments and reducing the administrative burden on healthcare professionals.
What changes can patients expect regarding prior authorization in the coming years?
Patients can expect significant improvements in the prior authorization process in the coming years, as insurers commit to implementing standardized electronic submission methods and timely responses for requests. By early 2027, it is anticipated that 80% of electronic prior authorizations will receive real-time approvals, enhancing the overall patient care experience and reducing waiting times for necessary medical services.
Why do some criticize the prior authorization process in U.S. healthcare?
Critics argue that the prior authorization process often leads to delays in critical patient care and increases administrative burdens for healthcare providers. Many healthcare professionals believe that the requirements for prior authorization can contribute to physician burnout and impede the timely delivery of necessary treatments, ultimately affecting patient outcomes.
What role does prior authorization play in patient care improvement initiatives?
Prior authorization plays a significant role in patient care improvement initiatives by ensuring that necessary care is provided while also managing healthcare costs. However, with recent reforms aiming to simplify this process, insurers hope to balance the need for cost control with the need to facilitate prompt access to care, enhancing the patient experience and outcomes.
How will changes to prior authorization affect access to healthcare for 257 million Americans?
The changes to prior authorization processes implemented by major health insurers are expected to improve access to healthcare for approximately 257 million Americans by expediting approval processes and reducing unnecessary barriers. These reform measures aim to link patients to the care they need more swiftly, thus improving the overall efficiency of the U.S. healthcare system.
What specific measures are being taken to simplify the insurance approval process for healthcare providers?
Health insurers are taking specific measures to simplify the insurance approval process by standardizing electronic prior authorization submission methods, reducing the types of claims that require prior authorization, and ensuring quicker response times for approvals. These initiatives aim to alleviate the administrative strain on healthcare providers and enhance patient access to necessary treatments.
What impact did public outcry have on reforms to the prior authorization process?
Public outcry regarding the challenges and delays imposed by the prior authorization process has led to increased scrutiny of the U.S. health insurance industry, prompting major insurers to commit to reforms. These changes aim to streamline the approval process and ultimately improve patient care, responding to the demand for a more efficient healthcare system.
| Key Point | Details |
|---|---|
| Commitment from Insurers | Major U.S. health insurers like CVS Health, UnitedHealthcare, and Cigna are making voluntary commitments to expedite prior authorizations. |
| Impact on Patients | This initiative aims to benefit 257 million Americans by reducing delays in care, denials, and administrative burdens on healthcare providers. |
| Criticism of Prior Authorization | Prior authorization often delays care and contributes to physician burnout, with critics arguing it complicates rather than simplifies care delivery. |
| Standardization Initiatives | The insurers plan to implement standardized methods for submitting electronic prior authorization requests by early 2027. |
| Future Developments | By 2026, insurers will limit claims requiring prior authorization, making the process more manageable for healthcare providers. |
Summary
Prior authorization is an essential aspect of the U.S. healthcare system, with major insurers taking steps to streamline the process. Recent commitments by companies such as CVS Health and UnitedHealthcare aim to simplify this often controversial procedure, enhancing patient care efficiency for millions. By reducing the burdens associated with prior authorization, these efforts seek to address the growing concerns around care delays and administrative overwhelm faced by healthcare providers. As these changes roll out, they promise to transform the prior authorization landscape, ensuring quicker access to necessary medical services.