Trump Rejects Medicare Coverage for Obesity Drugs Proposal
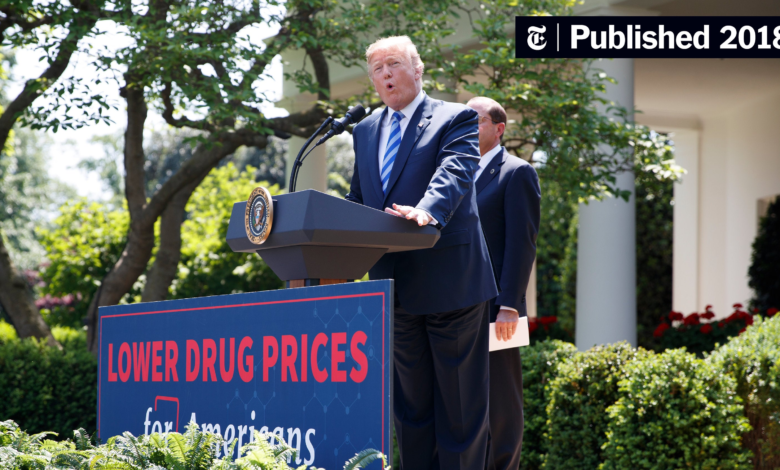
In a significant move, Trump rejects Medicare coverage for obesity drugs, turning down a proposal set forth by the Biden administration. This decision influences access to critical weight loss treatments like Wegovy and Zepbound, which many Americans rely on. Although the Centers for Medicare and Medicaid Services hinted at future evaluations of this coverage, immediate action halts expanded availability. The proposed Medicare coverage would have opened doors for millions suffering from obesity, a condition that exerts heavy influence on healthcare costs nationwide. As obesity treatment drugs, such as Wegovy and Zepbound, come with towering price tags often exceeding $1,000, many individuals face financial hurdles without insurance support.
In a notable rejection of healthcare reform, Trump has turned away a Biden initiative aimed at expanding Medicare’s coverage for weight management pharmaceuticals. This proposal, which could have transformed access to contemporary obesity treatments, prominently featured drugs like Wegovy and Zepbound, designed to aid individuals struggling with weight loss. By not supporting this coverage, the administration may shape the landscape of healthcare affordability for those classified as obese, defined by a BMI of 30 or higher. As the cost of these therapies could reach $35 billion over the next nine years, the debate over Medicare obesity drug costs looms large. The current landscape finds many left to grapple with the high expenses of critical obesity treatment drugs without the backing of federal assistance.
Trump Rejects Biden Medicare Proposal for Obesity Drug Coverage
In a significant political move, President Donald Trump has firmly rejected the Biden administration’s proposal to have Medicare cover revolutionary obesity treatment drugs such as Wegovy and Zepbound. This decision comes alongside a growing debate regarding healthcare policies and expenditures in the United States. The Biden Medicare proposal sought to enhance accessibility and affordability of these obesity drugs for millions suffering from weight-related health issues, but Trump’s administration has prioritized fiscal conservatism, worrying about the potential costs that could exceed $35 billion over nine years.
The ramifications of Trump’s rejection could have substantial implications for patients who rely on these medications for weight loss and related health benefits. Currently, obesity treatments are often not covered by Medicare, leaving many Americans to grapple with the high costs. Drugs like Wegovy and Zepbound, which can cost around $1,000 without coverage, pose significant financial barriers. As the debate unfolds, the Centers for Medicare and Medicaid Services have hinted at potential future reconsiderations of drug coverage, keeping hope alive for patients in need.
Understanding Wegovy and Zepbound: Implications for Obesity Treatment
Wegovy and Zepbound are part of a new generation of obesity medications that have shown promising results in clinical settings. Designed to support weight loss efforts in adults classified as obese, these drugs work by mimicking gut hormones that regulate appetite, leading to significant decreases in body weight. The Biden Medicare proposal aimed to include these groundbreaking treatments in their coverage, recognizing the importance of pharmacological assistance in managing obesity, which is a growing public health concern.
Without Medicare coverage, the utilization of these drugs remains limited to those who can afford them out-of-pocket, effectively excluding many lower-income patients from receiving potentially life-changing treatment. Furthermore, with a rising prevalence of obesity, ensuring greater access to effective treatment options through Medicare could transform healthcare outcomes significantly. The controversy surrounding Trump’s rejection of the proposal not only highlights the clash of political ideologies but also raises questions about the moral responsibility of the government to address an epidemic affecting millions.
The Economic Debate Surrounding Obesity Drug Coverage
The economic implications of the Biden administration’s proposal to include obesity drugs in Medicare coverage cannot be overstated. With estimates suggesting that such coverage could cost up to $35 billion over a decade, critics argue that this could unfavorably strain the Medicare system. Proponents, however, advocate for the long-term cost savings that could stem from improved health outcomes and reduced healthcare costs associated with obesity-related comorbidities, such as type 2 diabetes and heart disease.
Determining whether to invest in obesity treatment drugs via Medicare requires a careful examination of the benefits versus the projected financial burden. While the upfront costs are significant, the potential economic savings from preventing severe health complications make it a topic worthy of debate. As the government navigates these considerations, stakeholders must balance the urgent needs of patients with responsible fiscal management to create an effective and sustainable healthcare model.
The Future of Obesity Treatment in Medicare
The future of obesity treatment within the Medicare framework remains uncertain following Trump’s rejection of the Biden Medicare proposal. However, the Centers for Medicare and Medicaid Services may reconsider this decision as the healthcare landscape evolves. As awareness of obesity as a chronic disease grows, pressure mounts on policymakers to prioritize treatment options within Medicare coverage, especially for populations at risk due to obesity-related health conditions.
Looking ahead, ongoing discussions about healthcare reform and obesity management strategies will be critical. As more individuals seek effective obesity treatments, the question will remain: how can Medicare adapt to include innovative drugs like Wegovy and Zepbound? Finding a balance between economic feasibility and patient access may pave the way for a more inclusive approach to obesity treatment under Medicare in the future.
Obesity Drug Accessibility: A Socioeconomic Issue
The accessibility of obesity drugs like Wegovy and Zepbound transcends mere healthcare policy; it reflects broader socioeconomic issues affecting millions of Americans. Individuals from lower-income backgrounds often struggle to access these essential obesity treatments due to the high costs associated with such medications. Without Medicare’s support, many find themselves unable to afford these treatments, which could lead to severe health complications related to obesity, further exacerbating health disparities.
This situation underscores the need for a more equitable healthcare system that provides adequate coverage for essential medical treatments. Policymakers must grapple with the implications of not providing necessary resources to individuals suffering from obesity, which is not just a personal health issue but a societal one. Bridging the gap between socioeconomic status and access to effective healthcare solutions will be vital in the coming years.
Public Health Implications of Rejecting Obesity Drug Coverage
The public health ramifications of Trump’s rejection of Medicare coverage for obesity drugs are profound. Widespread availability of effective obesity treatments could significantly decrease the burden of obesity-related diseases, improving overall health outcomes within the population. However, without this coverage, many Americans may continue to suffer in silence, unable to access the care they need to combat their obesity and its associated health risks.
Moreover, the decision could lead to a phenomena known as ‘treatment desert,’ where patients who require medication cannot obtain it due to financial constraints, further complicating efforts to manage obesity on a national scale. Experts argue that addressing obesity is one of the keys to improving public health, particularly given its connections to various chronic illnesses. The rejection of coverage not only impacts individual patients but also has serious implications for healthcare costs and overall population health.
Political Dynamics Behind Healthcare Decisions
The political undercurrents influencing healthcare decisions are multifaceted, particularly in the context of Trump’s rejection of the Biden administration’s proposal for Medicare to cover obesity drugs. This decision elucidates the partisan divide concerning health policy and the role of government in providing essential medications. Trump’s administration prioritizing cost-cutting measures reflects a broader skepticism of government spending in healthcare, which often clashes with the Democratic perspective that emphasizes expanded coverage and access to necessary medical treatments.
These political dynamics can significantly impede progress in addressing time-sensitive health issues like obesity. The challenge lies in finding common ground that allows for effective healthcare solutions while managing the economic realities of government budgeting. As the healthcare discourse continues, it will be essential for all political parties to recognize the moral imperative of addressing public health challenges, particularly those with widespread implications such as obesity.
Lessons from Other Countries on Obesity Drug Coverage
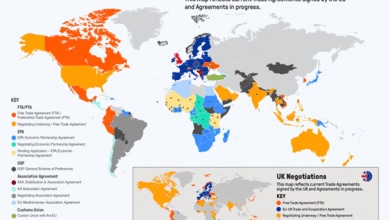
Around the world, different healthcare systems have approached the issue of obesity treatment in varied ways. Countries like Canada and those in Europe often provide broader coverage for obesity medications, recognizing the long-term benefits of preventing chronic diseases associated with obesity. As the United States grapples with its healthcare challenges, looking at successes and setbacks in other countries could offer valuable insights into the potential effects of Medicare coverage for obesity drugs like Wegovy and Zepbound.
These international examples showcase the importance of viewing obesity not merely as a personal failing but as a public health concern that warrants comprehensive treatment strategies. Adopting a more inclusive approach to covering essential medications could not only improve health outcomes but also alleviate the financial burden on the healthcare system by reducing the prevalence of chronic conditions linked to obesity.
The Role of Advocacy in Healthcare Policy Changes
Advocacy plays a crucial role in shaping healthcare policy, especially concerning critical issues like obesity drug coverage. Organizations and community groups work tirelessly to promote awareness of the importance of access to effective treatments like Wegovy and Zepbound. Their efforts are essential in pressing lawmakers to reconsider policies that may hinder accessibility to necessary medical interventions, especially for vulnerable populations suffering from obesity.
As public advocacy continues to grow, there is potential for shifts in policy that prioritize patient needs and health equity. Grassroots movements and campaigns that highlight personal stories can shift public perception and influence legislative outcomes, ensuring that the voices of those affected by obesity are heard in political discussions. Amplifying these narratives is vital in pushing for Medicare to cover obesity treatments, highlighting the essential role of advocacy in healthcare reform.
Frequently Asked Questions
Why did Trump reject Biden’s proposal for Medicare to cover obesity drugs like Wegovy and Zepbound?
Trump rejected the Biden administration’s proposal to cover obesity drugs, including Wegovy and Zepbound, primarily due to concerns over the significant costs to the government, estimated at around $35 billion over nine years. This decision impacts millions of Americans who might benefit from these treatments.
What are the implications of Trump’s rejection of Medicare coverage for obesity treatment drugs?
The rejection of Medicare coverage for obesity treatment drugs like Wegovy and Zepbound means that many patients will continue to face high out-of-pocket costs for these medications, which can exceed $1,000 per month. This may limit access to these essential treatments for those who are classified as obese.
Could Medicare coverage for obesity drugs like Wegovy and Zepbound be reconsidered in the future?
Yes, the Centers for Medicare and Medicaid Services suggested that coverage for obesity drugs like Wegovy and Zepbound might be reevaluated in the future. This leaves a possibility for changes in policy depending on future administrative priorities.
How do Wegovy and Zepbound relate to Trump’s rejection of Medicare’s obesity drug coverage?
Wegovy and Zepbound are specific GLP-1 medications targeted by the rejected Biden Medicare proposal. Trump’s decision not to expand Medicare coverage to these drugs reflects ongoing debates about healthcare costs and access to obesity treatments.
What criteria would have been used for Medicare coverage of obesity drugs under the Biden proposal?
Under Biden’s proposal for Medicare to cover obesity drugs, only individuals with a body mass index (BMI) of 30 or higher would qualify for coverage. This targeted those classified as obese, who might benefit most from treatment like Wegovy and Zepbound.
How does Trump’s rejection affect the cost of obesity drug treatments for Medicare patients?
Trump’s rejection of Medicare coverage for obesity drug treatments like Wegovy and Zepbound keeps the financial burden on patients, as they will likely have to continue paying the full retail prices for these medications, which are substantial.
What are the alternatives for Medicare recipients seeking coverage for obesity treatment drugs?
Currently, some Medicare recipients may obtain coverage for obesity treatment drugs like Wegovy and Zepbound if they have certain medical conditions such as diabetes or heart risks. However, the broader access proposed by the Biden plan is not in effect due to Trump’s rejection.
What is the public response to Trump rejecting Medicare coverage for obesity drugs?
The public response to Trump’s rejection of Medicare coverage for obesity drugs has been mixed, with concerns raised about access to necessary treatments for obesity and the associated healthcare costs faced by individuals without adequate insurance.
| Key Point | Details |
|---|---|
| Proposal Rejected | Trump rejected the Biden administration proposal for Medicare to cover obesity drugs like Wegovy and Zepbound. |
| Future Consideration | CMS may reconsider coverage for these drugs in the future. |
| Cost Implications | The proposal could have cost the government around $35 billion over nine years. |
| Current Coverage | Currently, most health insurance plans, including Medicare, do not cover weight loss treatments. |
| Eligibility | Only individuals classified with a BMI of 30 or higher would qualify for coverage under the proposal. |
| Stock Market Impact | Stock prices for Eli Lilly and Novo Nordisk dropped following Trump’s announcement. |
Summary
Trump rejects Medicare coverage for obesity drugs, impacting access for millions. The recent decision halts the Biden administration’s proposal aimed at including essential weight-loss medications like Wegovy and Zepbound under Medicare’s coverage umbrella. While this could have facilitated treatment for those struggling with obesity, it also posed significant financial implications for the government, estimated at $35 billion over nine years. Though there is potential for future reconsideration by the Centers for Medicare and Medicaid Services, currently, many patients will continue to face hurdles in accessing these expensive treatments without adequate insurance support.